Over 80% of patients in the acute phase of stroke (ischemic and hemorrhagic) have hypertension at the time of arrival at the emergency (> 140/90), different factors cause an “immediate” hypertension (anxiety, pain,intracranial hypertension …) The stroke itself responsible for secondary hypertension (in response to ischemic and hemorrhagic vascular occlusion to increase intracranial pressure, PIC) and chronic hypertension (common to the patient and premorbid). Possibly the latter may be partly responsible for the stroke but represents just over 50% of cases.
Will only be present hypertension in 60% of patients at discharge and therefore the remaining 30% were reactive or secondary to acute-subacute phase of stroke.
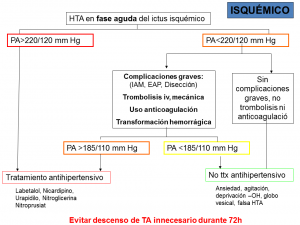
It is important in the acute phase of ischemic stroke avoid a sudden drop in blood pressure since much of the ischemic tissue presents a failure of cerebral autoregulation, no vascular tone function as vessels act like rigid tube where perfusion through it depends exclusively on the mean arterial pressure.
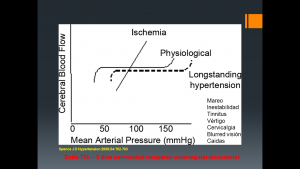
In this acute phase of stroke can not maintain a continuous perfusion pressure “plateau-line graphic green” despite continuing daily oscillations of blood pressure. It becomes a continuous “red slope-line graphic” brain pefusion proportional to the mean arterial blood pressure line .
If you also add some vascular occlusion unreasonably important lowering blood pressure can get irreversible tissue damage and even potentially salvageable ischemic penumbra. Hence the limits of handling high levels of blood pressure in acute stroke.
Apparently this dramatic situation lasts between 48-72 hours self after stroke. In fact some objective in acute phase curve “J” or “U”. In turn excess blood pressure above 220/120 may be associated with bleeding in case of cerebral edema or reperfusion.
Therefore if we indicate tPA treatment, thrombectomy, endarteectomy or some kind of cerebral revascularization these limits blood pressure 185/110 shall be lowered to a ceiling (some recommendation 185/105). Next 48-72 hours as the rest should be valued the gradual decline until TA 160/100 and 140/90 gradually to normal limits. Hypertensive emergency cases with involvement as aortic dissection, myocardial infarction, acute lung edema … may imperative lower these limits even in the acute phase quickly.
In the acute phase of hemorrhagic stroke hypertension is the variable that we can get better control to prevent rebleeding or clinical worsening. TA maximum limits are 185/105, although it is increasingly more aware of these limits if hematomas secondary to hypertension as deep or basal ganglia are excessive. We accept lower BP below 160/100 acute phase and try to normalize h below 48 140-90 (has not been shown that there is penumbra around hematoma, but rather edema may worsen with hypertension). In lobar or large hematomas it is true that the limits might be the same, but if we consider an increase in intracranial pressure (ICP) may lower BP to these limits apart from being difficult can be harmful because they are aborting one compensatory response to maintain cerebral perfusion pressure to counteract the increased intracranial pressure.
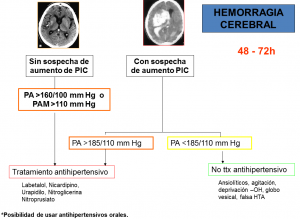
Recent studies such as INTERACT II, ATTACH II have provided evidence and proof of concept that a limit of BP below 140/90 mmHg is beneficial in most cases of cerebral hematoma without extreme increases of ICP. No need to wait in most cases to have figures of 185/105 to start treating hypertension.